Rowland Payne Syndrome: An In-Depth Review
Rowland Payne Syndrome | 28 April 2025
Rowland Payne Syndrome (RPS) is a rare but clinically significant neurological syndrome first described in 1981 by Dr. Rowland Payne. It presents with a distinct triad of clinical features: ipsilateral Horner’s syndrome, phrenic nerve palsy, and vocal cord paralysis, typically resulting from underlying malignancies, primarily breast cancer. As awareness of RPS grows, early diagnosis becomes critical for effective management and improved outcomes.
Understanding the Lymphatic and Nervous Systems
The lymphatic and nervous systems intersect at critical anatomical points in the body. The phrenic nerve, sympathetic trunk, and vagus nerve (or its branch, the recurrent laryngeal nerve) are located closely together near the thoracic inlet. Disruption at this anatomical site, often due to mass lesions such as metastatic cancer, results in the symptomatic triad characteristic of RPS.
Rowland Payne Syndrome “refers to a constellation of clinical signs caused by lesions affecting the sympathetic trunk, phrenic nerve, and recurrent laryngeal nerve” [Eyewiki, 2024].
Clinical Presentation and Diagnosis
Patients typically present with signs including:
– **Horner’s Syndrome**: Ptosis, miosis, and anhidrosis due to sympathetic trunk involvement.
– **Phrenic Nerve Palsy**: Leading to diaphragmatic paralysis and respiratory difficulties.
– **Vocal Cord Paralysis**: Resulting in hoarseness or dysphagia.
Other features may include brachial plexopathy, presenting as weakness or sensory deficits in the upper limb. A detailed neurological examination and patient history, particularly noting previous cancers, are critical.
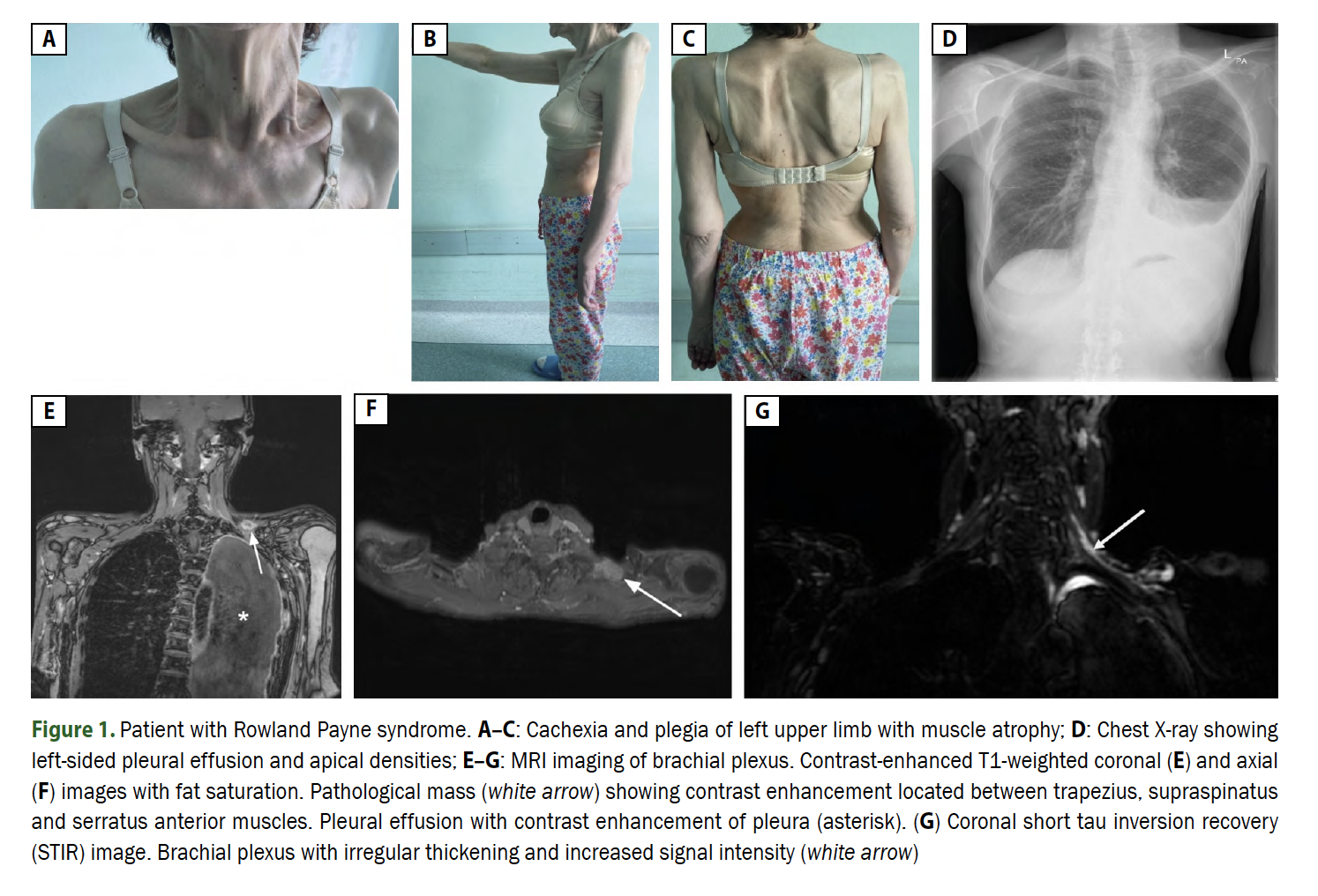
In a 2025 case study by Nieporęcki et al., a patient initially diagnosed with ALS exhibited signs of Rowland Payne Syndrome, including Horner’s syndrome, upper limb plegia, and cachexia. Detailed imaging and cytological examination confirmed breast cancer metastasis [Nieporęcki et al., 2025].
The diagnostic criteria, as per the Gold Coast guidelines for ALS, also help exclude mimicking conditions. In RPS, while some motor neuron signs may appear, the presence of sensory disturbances and focal symptoms aids differentiation [Nieporęcki et al., 2025].
Causes and Risk Factors
**Breast cancer** is the most commonly associated malignancy in RPS cases, although other neoplasms like lung carcinoma, anaplastic thyroid carcinoma, and neuroblastoma have also been implicated [Nieporęcki et al., 2025; PMC1439346]. Chronic exposure to carcinogenic factors, delayed cancer diagnosis, or recurrence after initial remission may all elevate risk.
Pathophysiology
The syndrome arises due to an expansive lesion in the anterior or inferior neck regions. The proximity of the phrenic nerve, sympathetic trunk, and recurrent laryngeal nerve means that a single mass can disrupt all three, leading to the classical triad of symptoms [PubMed: 7299783].
Mass effect or direct invasion results in:
– Interruption of sympathetic nerve fibers (Horner’s syndrome)
– Damage to the phrenic nerve (diaphragm paralysis)
– Impairment of recurrent laryngeal nerve (vocal cord paralysis)
Diagnostic Workup
A thorough workup typically includes:
– **Neurological Examination**: Focusing on cranial nerve function and limb strength.
– **Electrophysiological Studies**: EMG and nerve conduction studies to assess motor unit integrity.
– **Imaging**: MRI or CT scanning, especially targeted at the brachial plexus and thoracic inlet [Nieporęcki et al., 2025].
– **Cytological Analysis**: Pleural effusion or other biopsies to confirm malignancy.
In the landmark 2025 case, EMG revealed localized denervation, while MRI demonstrated a mass infiltrating the brachial plexus — crucial for distinguishing RPS from ALS or FOSMN (facial onset sensory and motor neuronopathy) [Nieporęcki et al., 2025].
Management and Treatment
The management of Rowland Payne Syndrome focuses primarily on addressing the underlying cause:
– **Oncological Treatment**: Chemotherapy, radiotherapy, or surgical excision based on tumor type and staging.
– **Symptomatic Management**: Respiratory support for phrenic nerve palsy; speech therapy for vocal cord paralysis.
– **Rehabilitation**: Physical therapy to maintain limb function.
Early identification and oncologic referral are vital. In many cases, particularly those involving metastatic breast cancer, prompt treatment significantly improves prognosis [Nieporęcki et al., 2025].
Prognosis
Prognosis varies depending on:
– The nature and aggressiveness of the primary tumor
– Timing of diagnosis
– Response to cancer therapy
While RPS often signals advanced malignancy, early detection and aggressive treatment of the underlying cancer can offer meaningful extensions to survival and quality of life [PMC1439346].
Importance of Differential Diagnosis
Rowland Payne Syndrome is frequently misdiagnosed as ALS due to overlapping motor neuron symptoms. However, several distinctions are key:
– Presence of sensory symptoms
– Localized EMG abnormalities
– Imaging findings of mass lesions
Clinicians should maintain a high index of suspicion, particularly in patients with previous cancer histories presenting with asymmetric motor deficits and cranial nerve involvement.
Notable Case Studies
**Case Study 1: Initial Misdiagnosis of ALS**
A 64-year-old woman with a history of breast cancer was initially diagnosed with ALS. Detailed evaluation revealed Horner’s syndrome, left phrenic nerve palsy, and brachial plexopathy, leading to the correct diagnosis of Rowland Payne Syndrome secondary to metastatic breast cancer [Nieporęcki et al., 2025].
**Case Study 2: RPS Secondary to Lung Carcinoma**
An earlier reported case involved a 65-year-old female whose first symptom was hemidiaphragm paralysis. Diagnosis revealed an underlying lung epidermoid carcinoma impacting the thoracic nerves [PMC1439346].
Research Gaps and Future Directions
Despite case reports, RPS remains under-recognized, leading to frequent misdiagnosis. Future research directions include:
– Enhanced imaging protocols to identify early nerve compression
– Biomarkers to differentiate between ALS and RPS
– Prospective studies assessing outcomes post-early intervention
Rowland Payne Syndrome is a rare, but diagnostically critical entity that underscores the importance of thorough neurological assessment and history-taking in patients with motor neuron disease symptoms. Early recognition and treatment not only improve neurological outcomes but also critically influence cancer management and overall survival.
As shown in clinical cases and ongoing studies, a multidisciplinary approach combining neurology, oncology, and radiology is the best path forward for patients with Rowland Payne Syndrome.
**References:**
– Eyewiki contributors. “Rowland Payne Syndrome.” Eyewiki. Accessed April 2025. [Link]
– Nieporęcki, K., et al. “Rowland Payne syndrome mimicking motor neuron disease.” Neurologia i Neurochirurgia Polska, 2025. [DOI:10.5603/pjnns.103859]
– Rowland LP, Payne R. “Horner’s syndrome with ipsilateral vocal cord and phrenic nerve palsies.” Postgrad Med J. 1981. [PubMed ID: 7299783]
– PMC1439346. “Rowland Payne Syndrome – Additional Case Studies.” National Library of Medicine.
– Amin R. Horner’s syndrome with ipsilateral vocal cord and phrenic nerve palsies. Postgrad Med J. 1984; 60(700): 140–142, doi: 10.1136/pgmj.60.700.140, indexed in Pubmed: 6709546.
– Kapoor V, Lodha R, Agarwala S. Superior mediastinal syndrome with Rowland-Payne syndrome: an unusual presentation of cervico-mediastinal neuroblastoma. Pediatr Blood Cancer. 2005; 44(3): 280–282, doi: 10.1002/pbc.20198, indexed in Pubmed: 15503296.
– Sierra-Hidalgo F, Aragón Revilla E. Rowland Payne syndrome. Neurologia (Engl Ed). 2021 [Epub ahead of print]; 36(9): 734–736, doi: 10.1016/j.nrleng.2021.02.002, indexed in Pubmed: 34266796.
